In 2018 it was reported that since the 1970s more than 78,000 chemicals have been approved for commercial use. Only 1,000 have been formally examined and considered for their carcinogenic potential - and of those the World Health Organisation consider 120 as ‘known’ carcinogens, 81 as probable carcinogens and 299 as possible carcinogens (i). See my previous blog at: https://myunexpectedguide.blogspot.com/2022/01/a-look-at-environmental-toxins.html
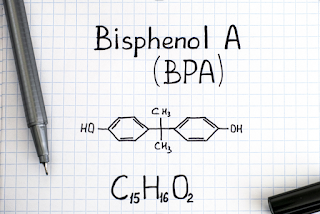
One of those chemicals which has been widely used is Bisphenol A (BPA) and it has been linked to cancer. It is a synthetic chemical used since the 1950s in making millions of plastics items including food packaging. By 2008 it was found in 93% of Americans urine. Research has linked it to cancers, hormone disruption and other serious health problems. It seems that when BPA enters the body it latches onto the body’s oestrogen receptors and tricks the body into thinking it’s oestrogen – thus increasing oestrogen levels for both men and women as well as disrupting the natural balance between our hormones. Not great stuff!A review in 2019 (ii) concluded; “Recent findings support a causal role of BPA at low levels in the development of cancers and in dictating their response to cytotoxic therapy.”
In 2020 a study (iii) found that people who had higher levels of bisphenol A in their urine were about 49% more likely to die during a 10-year period. Even as long ago as 1996 research was indicating concerns around endocrine disruption - sadly since then the list of endocrine disrupting chemicals (which includes BPA) has been steadily growing (iv).
Michael Greger of Nutrition Facts writes (2019)(v): “As the world’s oldest, largest, and most active organization devoted to research on hormones concluded, ‘even infinitesimally low levels of exposure—indeed, any level of exposure at all—may cause [problems].”
Not just plastics
A research review paper in 2018 (vi) noted: “Occurrence of BPA in breast and commercial milk represents a public health concern” and that “infants and children are particularly vulnerable to the effects of BPA exposure.”
While another 2018 report found that 93% of till receipts have BPA or bisphenol S (BPS) which were readily transferred onto the skin when handling them. Thankfully BPA has been banned in till receipts in the UK since January 2020. It seems BPS is still in some UK till receipts, although most major supermarkets are now using alternatives. So largely good news particularly for many shop workers who handle many till receipts in a day(vii).
Action on BPA – and alternatives
An EU ban on BPA in baby bottles only came into force in 2011 and in food packaging in 2020. It is hard trying to find out the extent of BPA use today; it is certainly being used in new products and of course in products that were made before the bans. Also while there are moves to reduce exposure to the public it seems there is little being done in terms of the impact on those workers, largely women, in the plastic industry.
Banning BPA may still lead to problems as in some cases it is being replaced by other unregulated chemicals like BPS which some argue could be worse than BPA.
BPS and bisphenol F (BPF) are the two most common replacements for BPA. Research in animals shows that both chemicals disrupt hormone balance comparably to-and sometimes worse than-BPA. Research also suggests that high levels of BPS may promote weight gain. The good news of the replacement BPS is that it may be less likely to leach into your food or beverage when heated in the container, as opposed to BPA, which is very sensitive to heat.
BPA-free does not mean chemical free. I have personally moved away from storing food in plastic where possible but many foods still arrive plastic wrapped especially supermarket products – even many of the organic ones are shrink wrapped. I remember that it was only a year ago that I came to understand that many canned foods had a BPA lining. I was horrified to find that research from the US in 2016 found that people who had consumed one can of food had 24% higher concentrations of BPA in their urine (within 24 hours after consumption) than people who had not consumed canned food.
Some companies have gone BPA free like Biona and some Mr Organic products – plus an increasing number of products can be found in jars for a price. However too many companies are not talking the issue seriously and it can be hard to find food labelled as to whether it is free from BPA, BPS or BPF - and of course this doesn’t answer the question about how safe the new liners are?
What can you do?
We don’t fully know the impact of the replacements so to avoid these chemicals in your food here’s a list that I’ve pulled together that may help us make better choices;
- if the container or plastic has a number 3 or 7 recycle code, it more likely contains BPA or BPS so that is one to avoid.
- Choose food and drinks packaged in glass rather than aluminium and plastics
- Tetra Pak - many non-dairy, beans and tomato products come in these and they are BPA and BPS free
- choose BPA-free cans where possible
- dried organic beans are less likely to be contaminated with chemicals than those from cans also sprouted beans can take much less time to cook
- use glass and stainless steel for food storage at home
- age increases the leaking of BPA from plastics so take care to throw away old or damaged plastic containers
- use bees wax wraps or other non-plastics to cover food
- never heat food in any type of plastic container
- silicone maybe safer than many plastics but has not been researched well and food-grade silicone can have many additives and colourings added which are not usually listed
- use a wooden shopping board; plastic has been shown to have more bacteria than wood and there is a risk of small plastic particles becoming dislodged and mixing with the food
- some takeaways are fine if you bring your own containers
- getting an organic box delivered or more regular shops at the farmers market could help reduce supermarket plastic wrapping
- avoid plastic coffee makers and if using filters use non-bleached paper
- Use unbleached parchment paper for baking and wrapping food. Parchment is often coated with silicone that is considered inert and safe; but as noted above research is limited
- Aluminum foil can be used to wrap foods but best used with dry foods; acidic foods like tomato sauce can increase the likelihood of it leaching into foods.
Do you have any suggestions to add to this list?
It’s worth noting again that we’ve have only looked at BPA here – as the 2018 report at the beginning of this blog suggests we need to look much wider – for example others like phthalates are also known to mimic and disrupt hormones while many others have other effects.
Notes
(i) ‘Anti Cancer Living’ by Dr Lorenzo Cohen and Alison Jefferies (2018)
(ii) https://pubmed.ncbi.nlm.nih.gov/30848227/
(iii) https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2769313
(iv) https://link.springer.com/article/10.1007/s11356-009-0107-7
(v) https://nutritionfacts.org/2019/11/05/why-hasnt-bisphenol-a-bpa-been-banned-completely/ and https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2726844
(vi) https://www.sciencedirect.com/science/article/abs/pii/S0278691518300863
(vii) https://saferchemicals.org/2018/01/17/new-report-9-out-of-10-receipts-contain-toxic-bpa-or-bps/
- dried organic beans are less likely to be contaminated with chemicals than those from cans also sprouted beans can take much less time to cook
- use glass and stainless steel for food storage at home
- age increases the leaking of BPA from plastics so take care to throw away old or damaged plastic containers
- use bees wax wraps or other non-plastics to cover food
- never heat food in any type of plastic container
- silicone maybe safer than many plastics but has not been researched well and food-grade silicone can have many additives and colourings added which are not usually listed
- use a wooden shopping board; plastic has been shown to have more bacteria than wood and there is a risk of small plastic particles becoming dislodged and mixing with the food
- some takeaways are fine if you bring your own containers
- getting an organic box delivered or more regular shops at the farmers market could help reduce supermarket plastic wrapping
- avoid plastic coffee makers and if using filters use non-bleached paper
- Use unbleached parchment paper for baking and wrapping food. Parchment is often coated with silicone that is considered inert and safe; but as noted above research is limited
- Aluminum foil can be used to wrap foods but best used with dry foods; acidic foods like tomato sauce can increase the likelihood of it leaching into foods.
Do you have any suggestions to add to this list?
It’s worth noting again that we’ve have only looked at BPA here – as the 2018 report at the beginning of this blog suggests we need to look much wider – for example others like phthalates are also known to mimic and disrupt hormones while many others have other effects.
Notes
(i) ‘Anti Cancer Living’ by Dr Lorenzo Cohen and Alison Jefferies (2018)
(ii) https://pubmed.ncbi.nlm.nih.gov/30848227/
(iii) https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2769313
(iv) https://link.springer.com/article/10.1007/s11356-009-0107-7
(v) https://nutritionfacts.org/2019/11/05/why-hasnt-bisphenol-a-bpa-been-banned-completely/ and https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2726844
(vi) https://www.sciencedirect.com/science/article/abs/pii/S0278691518300863
(vii) https://saferchemicals.org/2018/01/17/new-report-9-out-of-10-receipts-contain-toxic-bpa-or-bps/